Cystectomy
Cystectomy is a major surgical procedure involving the removal of the bladder and pelvic lymph nodes PLUS in males removal of the prostate gland and in females removal of the uterus and possibly ovaries. Cystectomy is most commonly performed to cure patients with invasive or recurrent high risk bladder cancer. Prior to surgery we will have ascertained the extent of disease by performing CT/MRI scans and possibly PET scans. Chemotherapy prior to surgery may be beneficial in eliminating any cancer cells that have already escaped from the bladder. Following removal of the bladder the urinary tract is reconstructed either by formation of a urostomy (ileal conduit) to drain urine into a bag applied to the skin or by formation of a 'neobladder' which drains urine via the urethra thus avoiding a urostomy.
Procedure
A general anaesthetic is administered often in conjunction with insertion of an epidural catheter to help with post operative pain relief. The anaesthetist will also insert an arterial line into your wrist (to monitor blood pressure and blood oxygenation during the surgery) and a central venous line into your neck to use as a route for drug and fluid administration.
A midline incision from the umbilicus to the pubic hair line is made. The connections of the bladder, prostate/uterus and lymph nodes to the body are controlled and divided.
Following complete removal of the bladder it is necessary to create a new urine drainage system. There are two main reconstructive options: an Ileal Conduit, or a Neobladder.
Ileal Conduit
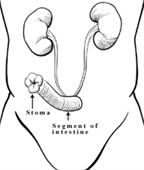
Fig. 1
An Ileal Conduit is the simplest type of urine diversion.
As shown in the diagram (Fig 1), the ureter pipes which carry urine from the kidneys are attached to one end of a segment of intestine; the other end of the intestine is brought up to the skin surface (to create a stoma) and the patient thereafter wears an external collection device ('bag') to collect urine.
The urostomy bag is emptied by an attached tap. The complete bag requires changing twice per week.
Surgery takes approximately 6 hours to perform. Blood loss is usually approximately 1L & blood transfusion required in approximately 50% of cases. Post-operatively you may stay in the intensive care unit for 1-2 nights for careful monitoring & nursing. Following this you return to the urology ward. Most patients are in hospital for 7-14 days.
Neobladder
Fig. 2
A Neobladder is a more complex type of reconstruction, it allows the patient to be free of a stoma - urine is passed via the urethra (Fig 2).
Fig. 4
The neobladder is constructed from 45-60cm of intestine. The intestine is cut and folded into a spherical shape and then the ureters from the kidneys and the urethra are attached to the neobladder (Fig 4).
Neobladder construction takes longer to perform than an ileal conduit.
Surgery takes approximately 7 hours to perform. Blood loss is usually approximately 1L & blood transfusion required in approximately 50% of cases. Post-operatively you may stay in the intensive care unit for 1-2 nights for careful monitoring & nursing. Following this you return to the urology ward. Most patients are in hospital for 7-14 days.
There will be a catheter draining the neobladder for approximately two weeks. It is flushed regularly with water to prevent mucus produced by the intestine from blocking the catheter. Before the catheter is removed x-ray dye is used to fill the Neobladder to ensure that it is watertight.
Once all catheters have been removed the Neobladder must be 'trained' so that the reservoir capacity can be increased to a capacity of 500ml. This process takes several months and during this time it is normal to have to wear pads to collect leakage of urine. Voiding (passing urine) from a neobladder is done by squeezing the abdominal muscles and relaxing the pelvic floor muscles; this requires some teaching and practice to learn. The community continence nurse will visit you regularly to help you with this.
Pre-Requisites
Several pre-requisites must be met before a patient is considered for this type of reconstruction. The patient must be in good general health, have good urine continence pre-operatively (no leakage), normal liver and kidney function, normal hand function and have no cancer in the urethra. Finally, the patient must be motivated to learn about living with a neobladder and be committed to long term follow-up. The final decision to proceed with a neobladder is made during the operation when the technical feasibility of the reconstruction and the presence of cancer in the urethra are both assessed.
Post-Operative Continence
Daytime continence (no pads) is recovered in 90% of men and 80% of women. Night time continence (continence while sleeping) is not as good; approximately 80% of patients are dry at night. During the night an alarm is set so that the Neobladder can be emptied once or twice; this helps prevent leakage at night.
In some patients (20%), complete neobladder emptying is not possible. These patients must then perform self catheterization (passing a small rubber catheter into the neobladder via the urethra) several times per day to empty the neobladder. Self catheterization is easy to learn and perform; patients are taught how to do this pre-operatively and must be prepared to accept the possibility of long term self catheterisation.
Metabolic Problems
Metabolic problems (problems with salt and water balance in the body) can occur due to reabsorption of body wastes present in urine. To prevent metabolic problems your urologist will advise that you take daily salt supplements and ural sachets in addition to a high fluid intake. This is particularly important during the first few months post-operatively when the risk of metabolic problems is greatest. Supplementation can usually be weaned off as the body adapts to the neobladder.
Nausea, vomiting and burning in the stomach are the common symptoms of metabolic upset; if these occur then urgent medical attention is required and you should contact your urologist and go to the nearest hospital to receive treatment.
Bowel Problems
Temporary post-operative diarrhea is common and is due to loss of the 40-60cm of intestine used to create the neobladder. If the diarrhoea does not improve then a bile salt binding agent such as Questran can be used. Vitamin B12 is absorbed through the part of the intestine used to create the neobladder. Loss of part of this intestine can lead to impaired absorption of certain vitamins including vitamin B12. Yearly vitamin B12 injections are recommended to prevent the possibility of a deficiency developing.
Pre-Cystectomy
Aspirin, clopidogrel, dabigatran, warfarin and any other blood thinning medications will need to be stopped prior to surgery. We will advise you on the timing of when to stop and re-start these medications.
A urine sample needs to be provided to the laboratory 1 week prior to surgery. Blood tests will be requested.
The stoma nurse will visit you to educate you on looking after a stoma and will mark the best location on your abdomen for the stoma - I place the stoma at this location.
Post Cystectomy
Delayed recovery of intestinal function is common following this surgery. This means that the intestines cannot push food and fluid through in a coordinated manner. This is called an 'ileus' and is characterised by loss of appetite, abdominal bloating, nausea and vomiting. A ileus will usually resolve spontaneously given enough time however this may take a week or more so during this time we may need to provide intravenous food in order to help your recovery.
Once your bowels begin to work again (passage of gas and bowel motions) then the ileus has resolved and you can resume a normal oral diet.
At least a third of patients experience a complication of some sort following this surgery which delays recovery. These complications usually relate to the intestine and may include intestinal obstruction, leakage from the bowel join up, infection, bleeding and blood clots. The risk of death as a result of a complication in the post operative period is approximately 3%.
Once you have resumed a normal diet, are comfortable and confident with management of the urostomy then you will head home. Th stoma nurse will see you regularly at home to help with the new stoma. If you have a neobladder then the continence nurse will see you. You will use a daily injection of a blood thinner for the first three weeks following surgery. This reduces the risk of blood clots developing.
Recovery of sexual function
Male: Surgery to remove the bladder prostate gland interferes with sexual function and reproductive ability- principally the ability to get and maintain an erection and always the permanent loss of ejaculation fluid. There may be penile shortening of 1cm or more, this is likely if nerves have been intentionally resected. It is however possible to have an orgasm without erection.
During surgery we often aim to preserve the fine nerves which control penile erection. These nerves run over the surface of the prostate gland as they pass to the blood vessels within the penis. These nerves are easily bruised and damaged during surgical removal. The likelihood of recovery of satisfactory function depends upon several factors: pre-operative sexual function, age, necessity for resection of the nerves and surgical experience and expertise in nerve preservation. Younger men with normal pre-existing erectile function who are suitable for nerve preservation and who have surgery by a surgeon experienced in nerve preservation are likely to recover reasonable function. There may be a 12 month period of relatively poor function before recovery occurs. I recommend early 'penile rehabilitation' for men wishing to resume sexual activity. This comprises regular induction of or enhancement of erections through oral or injectable drug therapy. Our clinic nurse will be able to instruct you in these techniques.
Female: Surgery to remove the bladder and uterus interferes with sexual function and reproductive ability - principally reduction of vaginal capacity, clitoral sensation and erection and vaginal lubrication.
In sexually active women we will discuss techniques to preserve vaginal capacity and overall sexual function such as preservation of the front wall of the vagina or the use of a skin and muscle graft into the vaginal wall to maintain capacity. This is done in conjunction with a plastic surgeon.
Return to work
Cystectomy is a major procedure & recovery from it is slow. Most patients will not be able to return to work for six weeks following surgery and this may be longer if there have been complications.
Follow up
I will see you daily during your hospitalisation then usually at 1 month then 3 to six monthly thereafter. Regular blood tests and radiological imaging will be performed.
I will telephone you when the surgical pathology report has been issued.
Other risks
Risks recognised as common or serious are listed below but this does not include the rare and extraordinary.
- Urinary infection
- Wound infection, dehiscence (wound re-opens) or herniation
- Cardiovascular and respiratory complications
- Stomal hernia