Bladder Reconstruction after Bladder Removal
Following complete removal of the bladder it is necessary to create a new urine drainage system. There are two main reconstructive options: an Ileal Conduit, or a Neobladder.
Ileal Conduit
Fig. 1
An Ileal Conduit is the simplest type of urine diversion.
As shown in the diagram (Fig. 1), the ureter pipes which carry urine from the kidneys are attached to one end of a segment of intestine; the other end of the intestine is brought up to the skin surface (to create a stoma) and the patient thereafter wears an external collection device (‘bag’) to collect urine.
Neobladder
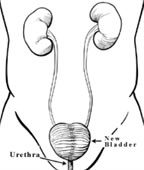
Fig. 2
A Neobladder is a more complex type of reconstruction, it allows the patient to be free of a stoma - urine is passed via the urethra (Fig. 2).
Fig. 4
After the bladder and pelvic lymph nodes have been removed the neobladder is constructed from 45-60cm of intestine. The intestine is cut and folded into a spherical shape and then the ureters from the kidneys and the urethra are attached to the neobladder (Fig. 4).
Surgery and Post Operative Care
Fig. 3
Surgery is performed via a 12cm incision beginning just below the belly button and continuing to the pubic hair line (Fig. 3).
Neobladder construction takes several hours longer to perform than an ileal conduit.
Post-operatively the patient returns to the ward. Oral intake of food and fluid is delayed until intestinal function returns and this usually takes several days.
There will be a catheter draining the neobladder. This remains in place for approximately two weeks. It is flushed regularly with water to prevent mucus produced by the intestine from blocking the catheter. Before the catheter is removed x-ray dye is used to fill the Neobladder to ensure that it is watertight.
Once all catheters have been removed the Neobladder must be ‘trained’ so that the reservoir capacity can be increased to a capacity of 500ml. This process takes several months and during this time it is normal to have to wear pads to collect leakage of urine. Voiding (passing urine) from a neobladder is done by squeezing the abdominal muscles and relaxing the pelvic floor muscles; this requires some teaching and practice to learn. The community continence nurse will visit you regularly to help you with this.
Pre-Requisites
Several pre-requisites must be met before a patient is considered for this type of reconstruction. The patient must be in good general health, have good urine continence pre-operatively (no leakage), normal liver and kidney function, normal hand function and have no cancer in the urethra. Finally, the patient must be motivated to learn about living with a neobladder and be committed to long term follow-up. The final decision to proceed with a neobladder is made during the operation when the technical feasibility of the reconstruction and the presence of cancer in the urethra are both assessed.
Post-Operative Continence
Daytime continence (no pads) is recovered in 90% of men and 80% of women. Night time continence (continence while sleeping) is not as good; approximately 80% of patients are dry at night. During the night an alarm is set so that the Neobladder can be emptied once or twice; this helps prevent leakage at night.
In some patients (20%), complete neobladder emptying is not possible. These patients must then perform self catheterization (passing a small rubber catheter into the neobladder via the urethra) several times per day to empty the neobladder. Self catheterization is easy to learn and perform; patients are taught how to do this pre-operatively and must be prepared to accept the possibility of long term self catheterisation.
Metabolic Problems
Metabolic problems (problems with salt and water balance in the body) can occur due to reabsorption of body wastes present in urine. To prevent metabolic problems your urologist will advise that you take daily salt supplements and ural sachets in addition to a high fluid intake. This is particularly important during the first few months post-operatively when the risk of metabolic problems is greatest. Supplementation can usually be weaned off as the body adapts to the neobladder.
Nausea, vomiting and burning in the stomach are the common symptoms of metabolic upset; if these occur then urgent medical attention is required and you should contact your urologist and go to the nearest hospital to receive treatment.
Bowel Problems
Temporary post-operative diarrhea is common and is due to loss of the 40-60cm of intestine used to create the neobladder. If the diarrhoea does not improve then a bile salt binding agent such as Questran can be used.
Vitamin B12 is absorbed through the part of the intestine used to create the neobladder. Loss of part of this intestine can lead to impaired absorption of certain vitamins including vitamin B12. Yearly vitamin B12 injections are recommended to prevent the possibility of a deficiency developing.
Follow-up
Follow-up is initially every three months then six monthly. At each of these visits the urologist checks for cancer recurrence and ensures that the neobladder and kidneys are functioning well. Follow up is life long.